Abstract
Introduction:
The prevalence of psychiatric illness is up to 35% in sickle cell disease (SCD) patients. Depression in chronically ill patients affects the quality of life and compliance with treatment and regular physician visits. Therefore, we sought to examine racial and gender-based differences in the prevalence of depression and anxiety in SCD.
Methods:
We investigated the National Inpatient Sample 2019 employing International Classification of Diseases-10 (ICD-10) codes to include adult SCD patients. Multivariate linear or logistic regression was used (for continuous and categorical variables, respectively). The confounders adjusted for in the regression models were: history of MI and stroke, coronary artery disease, sleep disorders, chronic pain disorders, smoking, alcohol, obesity, PTSD, sexual abuse, arthritis, and physical disability, in addition to patient and hospital-level variables. We used Stata, version 14.2, to perform analyses considering 2-sided P< 0.05 as statistically significant.
Results:
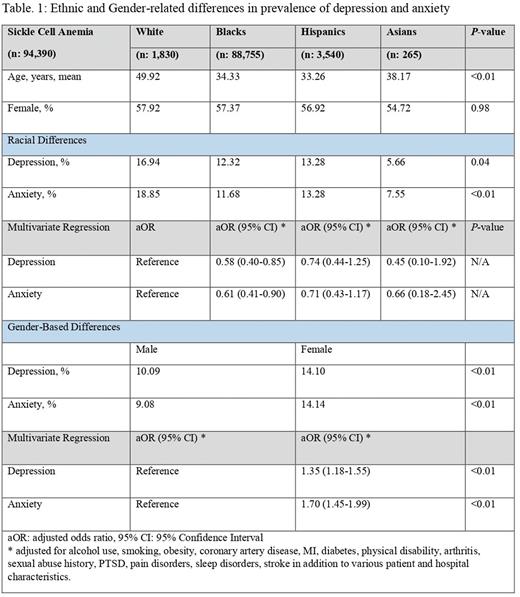
A total of 94,390 patients were included. 15,990 had depression, and 17,792 had anxiety. The prevalence of depression in various racial categories was: 16.94% in whites, 12.32% in blacks, 13.28% in Hispanics, and 5.66% in Asians (P=0.04). Anxiety prevalence was: 18.85% in whites, 11.68% in blacks, 13.28% in Hispanics, and 7.55% in Asians (P<0.01). On multivariate analysis, compared to whites, black had lower odds of depression and anxiety while Hispanics and Asians had similar odds (Table. 1). The prevalence of depression and anxiety in females was 14.10% and 14.12%, respectively. On multivariate analysis, compared to males, females had higher odds of the disease (adjusted odds ratio (aOR): 1.35, 95% confidence interval (CI): 1.18-1.55, P<0.01, and aOR: 1.70, 95% CI: 1.45-1.99, P<0.01, for depression and anxiety, respectively).
Conclusion:
Females and whites have higher rates of depression and anxiety compared to males and blacks with SCD. However, among racial minority groups other than blacks, the risk was similar to whites. Disease severity, social stigma, barriers in reporting, underdiagnosis, and genetic predisposition could contribute to these observed trends. Further research is needed to establish the factors responsible for these racial and gender differences.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal